To test or not to test: The science of community transmission, and why India might have left it too late
It’s not very comforting that the country's testing strategy is dictated by the availability of kits.
The COVID-19 pandemic has grown exponentially in the last few days and has now infected more than 3.75 lakh patients and killed about 16,362 in 195 countries. As of March 24, at least 536 cases have been detected in India, with about 107 and 95 cases in Maharashtra and Kerala, respectively. Around 15,24,266 passengers have been screened, and about 1,87,000 of them and their contacts are under community surveillance.
After the janta curfew on March 22, a nation-wide lockdown for 21 days was announced by Prime Minister Narendra Modi on Tuesday night.
While the Indian Council of Medical Research, in its press briefings, emphasises that India has still not reached the community transmission stage, many experts believe that we are just not testing enough to know that.
Pathology 101
Viruses are very sneaky and inconspicuous. They are invisible to regular microscopes and require powerful specialised electron microscopes. In most laboratory experiments, viruses are often identified by the carnage of dead bacterial and animal cells that they leave behind. This is why diagnosing viruses infections are so difficult.
The blue blob below is a human cell that has self-exploded (apoptosis) after being overwhelmed by SARS CoV-2 (red). To give you some context about the size, there are 30 trillion such blue cells in our body.

Patients infected by SARS-CoV-2 can be diagnosed by either directly looking for the virus or the body's response to the virus, like fever and antibodies.
Temperature screening
This is the first line of very non-specific testing that is done at airports to flag suspected COVID-19 cases. Fever is the body’s natural response in the face of an infection. It was reported in about 90 percent of the COVID-19 cases in China.
Temperature screening is typically done using thermal scanner cameras and non-contact infrared thermometers. The latter is more accurate. Although temperature screening is fast and accessible, it is not very reliable. Temperature gun only measures the temperature of the skin (face) and not the core body temperature. Despite a constant body temperature, a 10°C difference in air temperature can induce a 2°C change in the face temperature.
The median incubation time or the time from infection to the first symptoms is about five days but it may vary from one to 14 days. Therefore a lot of infected but asymptomatic travellers could simply pass through airport screening with normal temperatures. We’ll discuss more later in this article.
PCR
PCR, or polymerase chain reaction, is a test to directly detect the presence of viral genetic material. SARS CoV-2, the virus that causes COVID-19, stores its genetic material in the form of RNA, a close cousin of DNA. This genome of the SARS CoV-2 is essentially a manual that has instruction for virus production and transmission. Here is the complete genome of the virus that infected one of the first cases of COVID-19 in India. All organisms including viruses, bacteria, plants and humans have their own unique genomes. A human genome is typically 100,000 times bigger than that of SARS CoV-2.
In PCR, a small snippet of this genome, which is unique to the virus, is used. If the virus and, by proxy, its genome is present in the sample, then that small snippet makes multiple copies of itself, which is then used to confirm the presence of the virus. If there is no virus, the PCR snippet won’t multiply and a negative test will be shown.
SARS CoV-2 uses RNA; therefore, a slightly different version of PCR called Reverse Transcriptase (or RT-PCR) is used to diagnose it. The earlier version of this test was less efficient but newer versions approved by ICMR seem to have 100 percent sensitivity and specificity.
As of March 24, 22,694 samples from 21,804 individuals have been tested and 482 of these were positive for SARS CoV-2. In India, 104 government labs are operational, and 16 private labs have been approved for COVID-19 testing.
RT-PCR requires reagents, primers, probes, thermocyclers and many other different components. Probes are the rate-limiting aspect of COVID-19 testing in India. Because of this, the number of test kits available with the government is limited and so is their ability to widen the scope for testing.
CT scans have been the backbone of testing in China along with PCR. Ground glass opacities in the base and the periphery of the lungs is pretty specific to the CT scan of patients with COVID-19. But the disinfecting, operation and the availability of CT scan in India is another cause for concern. In early cases, however, neither CT scans nor PCR is sufficiently sensitive.
In response to infections, the human body produces specific pathogens neutralising molecules called antibodies. Antibody assays are less expensive and can provide additional insights like the stage of infection, and tell if someone has developed immunity after recovering for COVID-19. Several labs have successfully developed this test and right now are in the process of getting them validated.
After a patient recovers, the virus no longer exists in the nasopharyngeal swab and therefore PCR can’t detect it. But antibodies for the virus persist for a few months. Based on COVID-19 antibody prevalence in the population, these tests will also help us determine the true extent of this pandemic.
We are always behind
Every news channel passionately flashes the latest number of COVID-19 cases in India. But this reported number is not real-time. It’s like watching a cricket match. There is a few seconds of lag between the match and what you see on your screen. Similarly, every case that is reported was likely infected a week ago. It takes about 5-6 days for symptoms to manifest and a couple of days for PCR tests to confirm them. So the 50-odd cases that we had confirmed on March 24, were people who got infected a week ago. It will take another week before anyone really knows the number of people infected today.
Therefore, we are always behind.
This also means that we’ll find out if cases are subsiding only after a week. The graph below was prepared by the Chinese Center for Disease Control and Prevention. Look at the right end, while the actual number of infections that day (in blue) was decreasing, the number of cases reported (in orange) was high.

Parsimonious testing and the case for community transmission
We know that COVID-19 cases are introduced by infected travellers from affected countries. They are screened at Indian airports based on their temperature and symptoms. Symptomatic passengers are isolated and asymptomatics are put under community surveillance. These porous airport screenings — the only barrier between infected patients and our population — are hardly effective.
Studies have shown that patients with Ebola have slipped through despite thermal screening. One analysis by ECDC found that 75 percent of COVID-19 patients would be missed by thermal screening. More recent modelling has found that even in the best-case scenario, screening at airports can flag only half of all travellers with COVID-19.
It’s impossible to expect airport screening alone to stop the spread of COVID-19. Even if we track all the symptomatic cases, there is no way we can have the same success for asymptomatic cases. The ICMR, in its research paper on the modelling of the COVID-19 pandemic, notes: “Any containment strategy focused on symptomatic infections, no matter how comprehensively tends to be negated by the asymptomatic infections that escape detection and can go on to cause onward transmission in the community.”
Asymptomatic patients after screening are asked to quarantine themselves and are tracked by the Integrated Disease Surveillance Programme. Quarantined travellers who are tested positive or start to show symptoms are sent to isolation wards. But this strategy relies on the suspected cases cooperating. There have been several instances where people have evaded quarantine because of bad facilities at quarantine camps, fear, or sheer irresponsibility.
In that same ICMR analysis, with the best-case scenarios where the lower limit for virus transmissibility (R0=2, the relative infectiousness of asymptomatic cases as compared to symptomatic=0.1) is considered, and all symptomatic and 90 percent of the asymptomatic travellers are accounted for, the number of days to reach 1,000 cases — or an epidemic — is just 20 days. Again that’s the best case as compared to the worst, where 1,000 cases would be seen in less than a day if all asymptomatic patients are missed.
This modelling is only done on the arrivals from China and not other countries like Italy, the US, the UAE, and others. We now know from reports that most of our COVID-19 importation has come from non-China countries. For the best-case scenario, which buys sufficient time, 90 percent of asymptomatic patients would have to be identified. For this, the paper notes, “the only way to reach 90 percent diagnosis among asymptomatic arrivals may be through isolation and quarantine of all arrivals from specified origin airports. Resources may be better spent on the mitigation of infection in the community.”

The same paper also notes that before the airport screening started on January 15, 5,700 passengers had arrived from China. Of these passengers, 17 of them showed symptoms and were accordingly quarantined and hospitalised, while 885 arrivals could not be traced and their status remains unknown.
A recent study published in the journal Science estimates that undocumented cases (patients with very mild symptoms that are not reported as COVID-19 infection) were responsible for around 80 percent of all the recorded COVID-19 infection in China.
According to WHO, there are different stages to an outbreak depending on the status of transmission.
Imported cases only (Phase 1): all diagnosed cases were acquired outside the territory
Local transmission (Phase 2): all the cases can be accounted to imported cases and their contacts
Community transmission (Phase 3): cases which cannot be tracked back to any imported cases, their contacts or transmission chains and have an unknown or cryptic origin
About 80 percent of the COVID-19 patients would have mild symptoms. As asymptomatic patients with mild symptoms slip through airport screening and surveillance, community screening seems inevitable. Once a population proceeds in community transmission mode, it becomes increasingly difficult to control the epidemic.
But how do we know if we have reached community transmission yet? By testing suspected COVID-19 patients and determining if we can ascertain from them that they likely acquired the virus from here.
Here is where the problem starts.
Until March 20, ICMR only allowed healthcare workers, international passengers and their contacts to be tested. Anyone else outside this category with a potential community transmission-acquired infection could not be tested. This meant that ICMR’s guidelines only allowed for testing of imported and local transmission cases and not community transmission cases. It’s impossible to know if we are not looking!
ICMR’s line of argument is that we only test when finding evidence. To find evidence, they did a pilot study where 20 random samples of patients with acute respiratory distress but no travel or contact history from 50 VRDLs each would be tested for COVID-19. If a positive case turned up, the testing strategy would be broadened.
First, 826 samples turned out to be negative. While this plan sounds fine, it seems inadequate for a country the size of India. Most of the COVID-19 cases exhibit mild symptoms and are unlikely to have acute respiratory distress even if they acquired the virus through the community.
ICMR in their press briefing justified this by saying they have very limited PCR test kits and, therefore, they have to use it judiciously until more probes, the rate-limiting component, is acquired. But for a disease like COVID-19 with no cure, PCR tests are mostly relevant only in the early stage of the outbreak. If a patient comes with respiratory distress, doctors will provide them with supportive care like oxygen and mechanical ventilation. Something they would do to patients irrespective of COVID-19 or not, if they have pneumonia and ARDS (acute respiratory distress syndrome).
Testing serves a purpose mostly for isolation and contacting tracing in the early stages. Once we are neck-deep in this pandemic, those things just don’t matter that much. You test as many as you can and isolate everyone else who exhibits the symptoms of COVID-19. China did it when they reached 50,000 cases and New York City did it when they had 4,500. How can we control the early stage if we can’t even identify it? It’s not very comforting when India's testing strategy is dictated by the availability of kits.
ICMR recently changed its testing criteria to involve patients with severe acute respiratory infections (SARI) and has increased surveillance sites from 16 to 51. This symptomatic surveillance will definitely help in identifying community transmission. But did we miss any community transmission before this change? As we saw before, we’ll only know after a few days. Some reports indicate that India already has cases with unknown origin.
Despite thousands of cases, no country has reported community transmission to WHO yet.

A quick update on chloroquines
Chloroquine and Hydroxychloroquine are drugs that are regularly used for treating malarial infections. Both these drugs have become particularly popular because of their recent endorsement by Elon Musk and Donald Trump for COVID-19. Many have suggested that it should be taken prophylactically, or before exposure, as a preventive measure.
While they do seem to work in cell cultures in the laboratory, randomised-control trials in humans with COVID-19 would be necessary before such conclusions are drawn.
As of now, just a single human trial for hydroxychloroquine in Italy has been completed. While the results were optimistic, the methodology was shoddy and underpowered. Chinese researchers have claimed that chloroquine is effective against COVID-19 but are yet to share their data and results. Another small trial done in Shanghai, and China suggested that hydroxychloroquine was no better than placebo. Earlier experiments of chloroquine done for chikungunya virus exacerbated the infection instead of treating them.
On March 23, ICMR approved hydroxychloroquine as a prophylactic for health care workers treating COVID-19 patients and asymptomatic household contacts of lab-confirmed positive cases. Hydroxychloroquine requires a prescription but in a country like India where Schedule H drugs are carelessly sold over the counter, without adequate regulations, there will certainly be a lot of hoarding and profiteering as this information starts to drip unchecked in WhatsApp groups.
Along with malaria, Hydroxychloroquine is also used chronically by patients with lupus and arthritis. Unchecked self-medication for COVID-19 will also severely impact their access. Countries with COVID-19 have started to report chloroquine poisoning and death, which is straining an already burdened system.
SOLIDARITY and DISCOVER are two drug trials being conducted by the WHO and the European CDC. Results from their trials will hopefully bring more clarity about chloroquine’s efficacy. Till then, like most other things about this pandemic, we need to wait and watch.
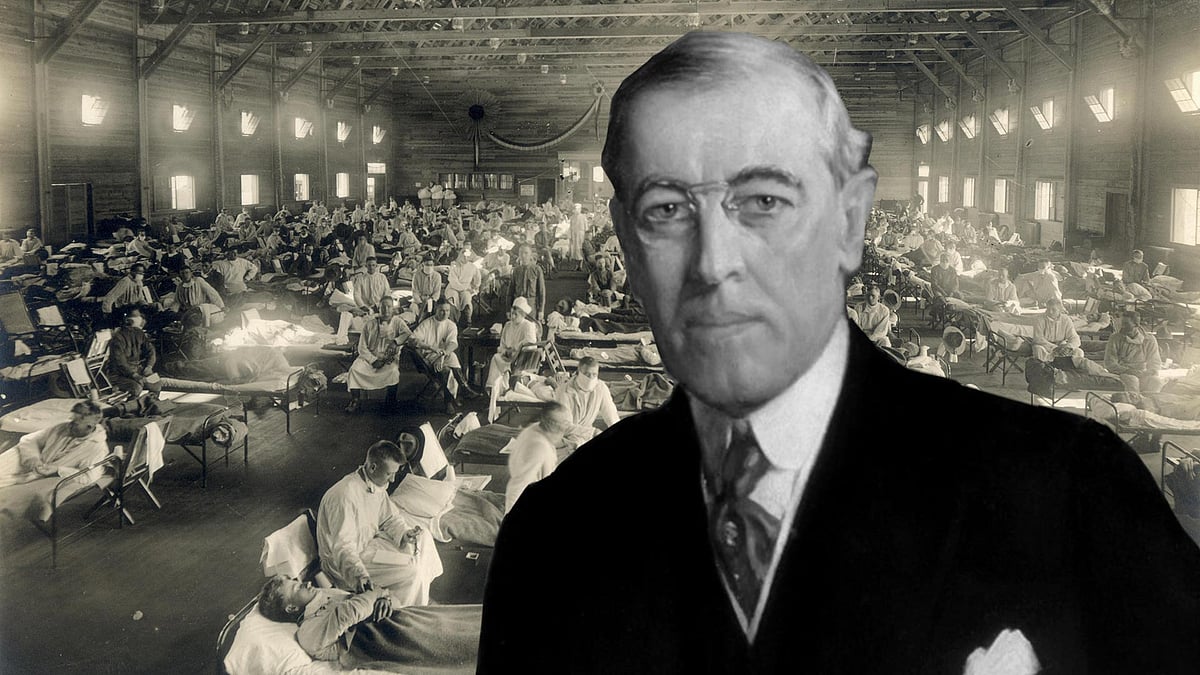 Spanish flu: How information policing and nationalist propaganda worsened a pandemic a century ago
Spanish flu: How information policing and nationalist propaganda worsened a pandemic a century ago Why India doesn’t seem to care about its poor even during a pandemic
Why India doesn’t seem to care about its poor even during a pandemic